
The Link Between Trauma and Teen Substance Use
Understanding Trauma in Adolescence
Trauma refers to intense stress or harm from distressing events that overwhelm a young person’s ability to cope.
These events can include abuse (physical, sexual, or emotional), witnessing violence (such as domestic or community violence), serious accidents or injuries, neglect or loss of a loved one, and other life-threatening or frightening experiences.
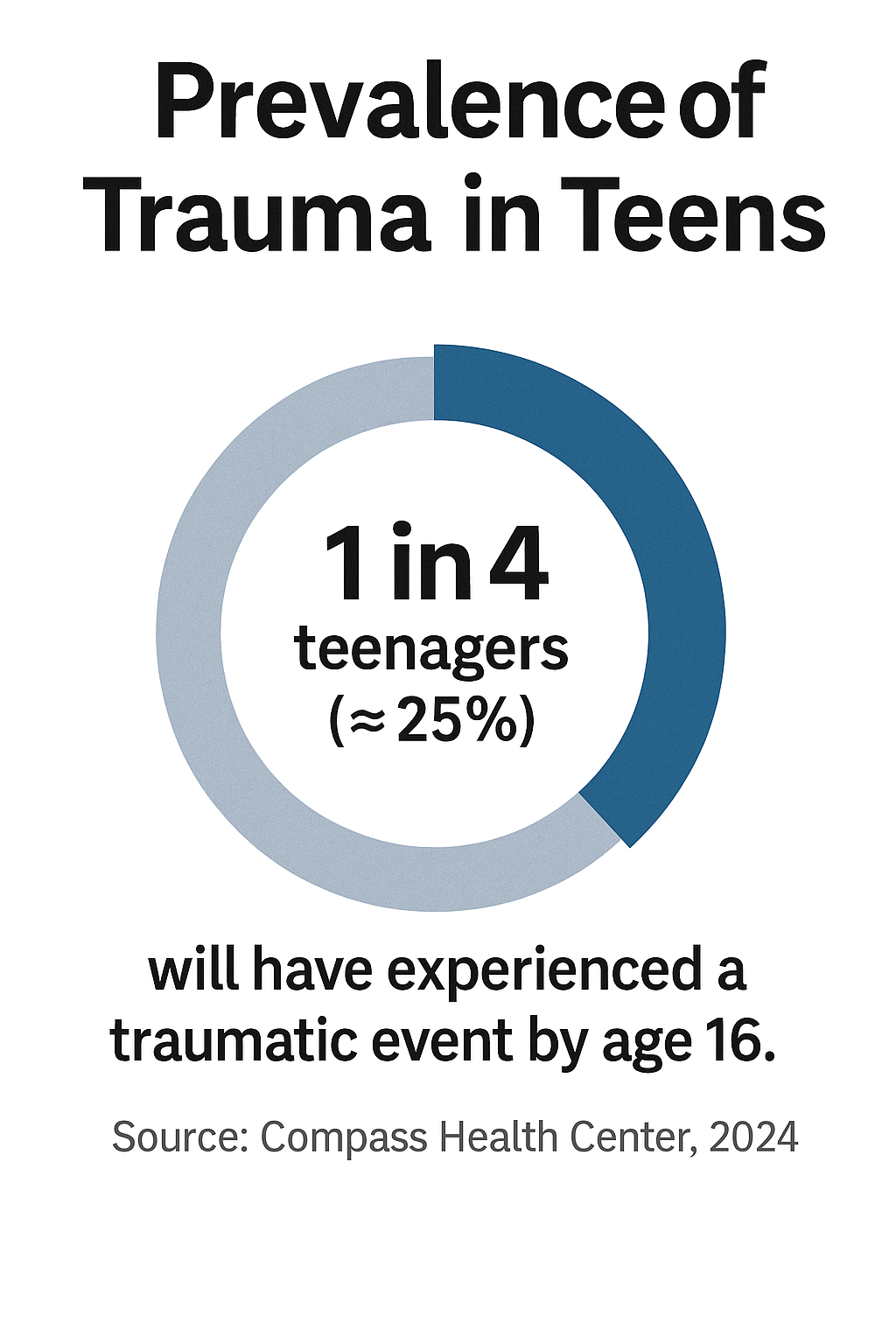
Unfortunately, such traumatic experiences are not rare in youth – national surveys indicate that about 1 in 4 children and adolescents will have been exposed to a traumatic event by age 16. Early-life trauma often leaves lasting emotional and biological impacts, and research consistently shows it is linked to a higher risk of behavioral health issues, including substance abuse.
In fact, traumatic experiences in childhood or adolescence are strongly associated with later substance use and the development of substance use disorders. Children and teens who go through trauma are particularly susceptible to developing addiction problems as they get older.
This link between trauma and teen substance use is a critical public health concern, as it affects a substantial number of youths and can have far-reaching consequences for their health, safety, and development.
Trauma as a Catalyst for Adolescent Substance Use
Experiencing trauma significantly increases the likelihood that a teenager will engage in substance use as a coping mechanism or path to relief. Multiple large-scale studies have documented this connection.
For example, a national survey of adolescents found that teens who had experienced **physical or sexual abuse or assault were about three times more likely to report past or current substance use compared to those with no history of trauma.
In other research, childhood trauma exposure has been linked to earlier and more frequent drug use in adolescence. One study of nearly 10,000 U.S. adolescents found that those who had experienced any potentially traumatic event before age 11 had significantly higher odds of illicit drug use – their likelihood of trying marijuana was about 1.5 times greater, and for cocaine nearly 2.8 times greater, than peers with no early trauma.
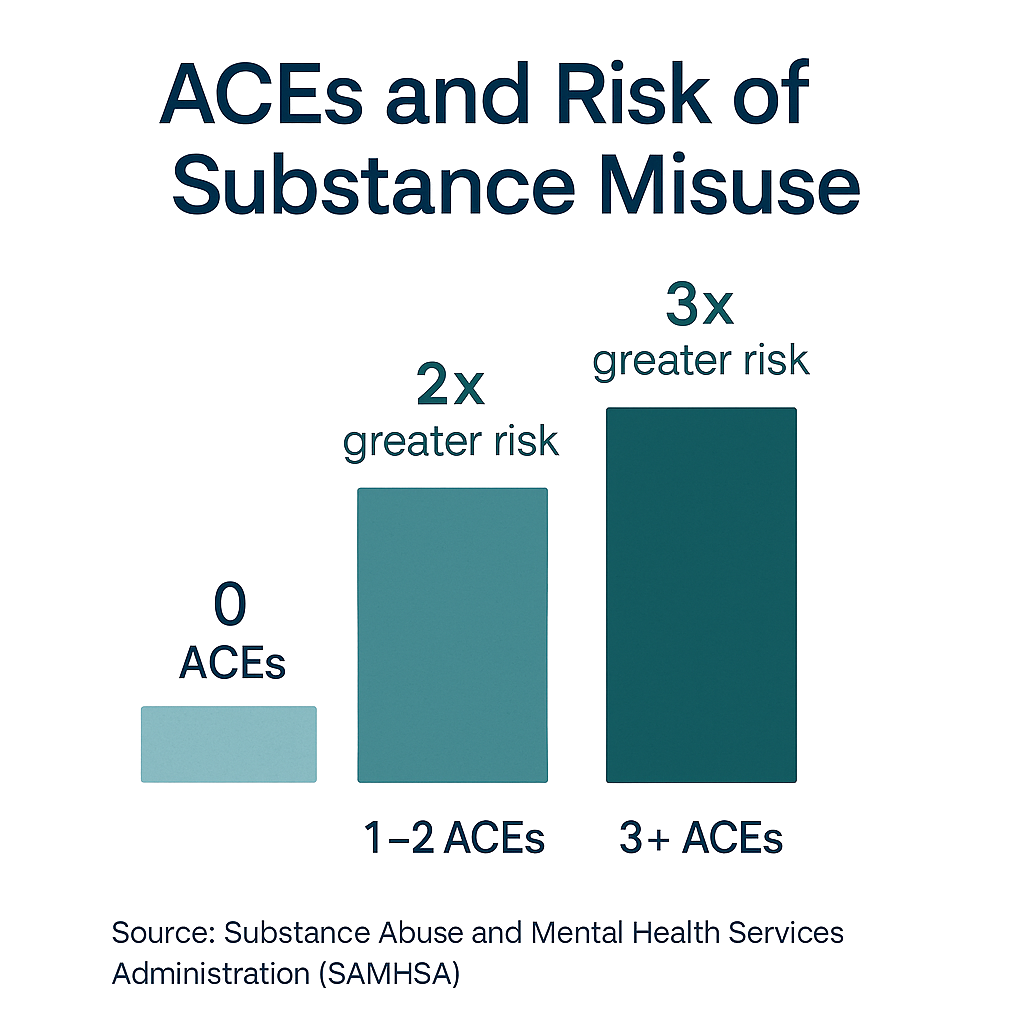
There is also a clear dose-response effect: the more traumatic experiences a teen has, the higher their risk of substance misuse. Data on Adverse Childhood Experiences (ACEs) – which measure cumulative trauma – show this vividly. According to a 2023 CDC youth behavior survey, high school students with four or more ACEs were over five times more likely to engage in heavy alcohol use and nearly nine times more likely to misuse prescription opioids, compared to students with no ACEs. Even having a moderate ACE score (2–3 traumatic experiences) almost doubled or tripled the risk of various substance use behaviors in teens. These statistics underscore that trauma is a potent catalyst for adolescent substance use.
Not only are traumatized teens more prone to start using substances, but a very high proportion of youth who develop serious substance problems have trauma in their backgrounds. Surveys of adolescents entering treatment for substance use disorders show that over 70% of these teens have a history of trauma exposure.

In other words, a majority of teens struggling with addiction have experienced at least one major traumatic event earlier in life. Furthermore, trauma-related mental health conditions often go hand-in-hand with youth substance abuse. For instance, post-traumatic stress disorder (PTSD) is commonly seen alongside teen addiction: multiple studies in North America have found that approximately 20% to 50% of adolescents with substance use disorders also meet criteria for PTSD.
The reverse is also striking – adolescents with PTSD or significant trauma symptoms are at elevated risk of developing substance use disorders; some estimates indicate up to 59% of youth who develop PTSD later develop substance abuse problems. This bidirectional overlap means trauma and addiction can reinforce each other in a vicious cycle, making early intervention all the more crucial.
Types of Traumatic Experiences Linked to Substance Misuse
While virtually any severe stressor can impact a teen, certain types of trauma are especially implicated in later substance use. Key examples include:
- Physical or Sexual Abuse: Suffering abuse in childhood dramatically raises the risk for addiction. In one survey of people with substance use disorders, almost half had a history of physical or sexual abuse. Those who experienced childhood physical abuse had about a 74% higher risk of developing a substance use disorder in their lifetime, and those with a history of childhood sexual abuse had a 73% higher risk. Such abuse is deeply traumatic and often leads adolescents to seek an escape or numbing through drugs or alcohol.
- Domestic Violence and Community Violence: Being the victim of violence or even witnessing violent events can trigger substance misuse. Teens exposed to interpersonal violence (e.g. witnessing domestic abuse or being in a violent environment) have an elevated likelihood of using drugs and progressing to addiction. Exposure to violence contributes to hyper-vigilance, anxiety, and fear, which some teens attempt to blunt with substances. Even broader traumatic events like acts of terrorism or school shootings have been associated with surges in youth alcohol, tobacco, and drug use in their aftermath. In short, violence-related trauma often primes adolescents toward substance use as a maladaptive coping strategy.
- Family Conflict, Loss, or Neglect: Chronic adversity in the family environment can be just as damaging. Parental conflict or divorce, the death of a parent, or living in a highly unstable, neglectful home all create severe stress that increases a young person’s vulnerability to substance use. For example, growing up with parental substance abuse or mental illness is considered an ACE that not only directly exposes a child to trauma, but also models substance use as a coping mechanism. A teenager who has lost a caregiver or endured ongoing family turmoil may turn to drugs or alcohol to self-soothe or escape a hostile home atmosphere.
- Discrimination and Bullying: Chronic stress from social trauma – such as racial discrimination, bullying, or stigmatization – can also drive adolescents toward substance misuse. Research indicates that experiencing prejudice or systemic discrimination causes toxic stress that raises the risk of substance use and misuse. Teens who feel marginalized or unsafe because of their identity or environment may use substances to cope with feelings of alienation, anger, or low self-worth stemming from these traumas.
- Serious Accidents or Injuries: Traumas that are physical in nature, like severe accidents, physical injuries, or life-threatening illnesses, have been linked to later drug and alcohol problems as well. A traumatic brain injury or other serious injury in childhood can disrupt brain regions responsible for decision-making and impulse control, making a teen more susceptible to addiction if they experiment with substances. Additionally, experiencing painful medical procedures or illnesses early on can introduce youths to opioids or other drugs, or leave psychological scars that they later attempt to numb with illicit substances. In sum, trauma can take many forms – from abuse and violence to loss, discrimination, or injury – and all of these dramatically increase an adolescent’s odds of substance use.
Why Trauma Drives Teens to Substance Use
Psychological Escape and Self-Medication:
The most immediate reason trauma can lead to substance use is that teens often use drugs or alcohol as a form of self-medication. Traumatic experiences frequently result in intense anxiety, depression, intrusive memories, or emotional pain.
Adolescents may discover that substances like alcohol, cannabis, or prescription sedatives temporarily numb their distress or dampen traumatic memories, providing a short-term escape from psychological pain. This self-medication hypothesis is well-established: young people who have experienced trauma turn to substances as a way to cope with overwhelming emotions and stress symptoms that they feel unable to handle otherwise.
For instance, an adolescent suffering from nightmares and hypervigilance after a violent assault might smoke marijuana or drink alcohol to induce relaxation and sleep. While these behaviors may bring fleeting relief, they ultimately worsen mental health and set the stage for dependency. The trauma is never truly resolved by substances – instead, substance use can compound a teen’s emotional turmoil by adding addiction, health problems, and new negative experiences on top of the original trauma.
Changes in the Brain’s Stress and Reward Systems:
Beyond the psychological drive to self-medicate, trauma in early life can actually rewire the developing brain in ways that make the struggle with addiction more likely. Adolescence is a critical period of brain development, and chronic traumatic stress can disrupt normal maturation of regions involved in stress response, impulse control, and reward processing.
Studies show that traumatic stress, especially when experienced in childhood or early adolescence, can cause lasting changes in brain function and behavior. Severe or prolonged stress floods the body with stress hormones and over-activates neural circuits related to fear and arousal. Over time, this can dysregulate the brain’s stress-response system (including the HPA axis) and sensitize the teen to future stress. Simultaneously, trauma affects key brain circuits for reward, motivation, and self-control.
Research supported by the National Institute on Drug Abuse finds that chronic trauma can increase craving-related neural activity and impair the brain’s ability to inhibit impulses. In practical terms, a traumatized adolescent may feel stronger urges to seek pleasure or relief (due to an overactive reward drive) and less ability to resist the temptation of drugs (due to weakened impulse control mechanisms). The neurobiological overlap between trauma and addiction is evident – the same brain systems that are thrown off balance by trauma are those hijacked by addictive substances.
Drugs like opioids or alcohol artificially stimulate the brain’s reward pathways and dampen stress, effectively “hitting the switch” that trauma has left malregulated. This is why early trauma exposure is associated with a greater likelihood of developing addiction later in life. Once addiction sets in, it can further exacerbate stress and trauma symptoms in a vicious cycle: for example, someone with trauma who becomes addicted to drugs might experience heightened PTSD flashbacks or anxiety during withdrawal, driving them to use again.
Trauma Triggers and Cravings:
Another insight from research is that trauma can directly make recovery harder by triggering cravings. Teens who have both trauma-related disorders and substance problems often report that reminders of their trauma (people, places, sensations associated with the event) can induce powerful urges to use drugs. Studies have documented that exposure to trauma reminders – say, the anniversary of a tragic event or returning to the location of an assault – spikes physiological stress and craving levels in individuals with co-occurring PTSD and SUD.
The substance provides a quick (but destructive) way to quell the spike in distress. This means that unless the underlying trauma is addressed, simply abstaining from substances can be exceedingly difficult for a teen – their environment or memories continually “trigger” the need to self-medicate. It also explains why relapse rates are high if treatment does not incorporate trauma-focused therapy.
Not Inevitable, But Significant:
It is important to note that not every teenager who experiences trauma will develop a substance use disorder. Many factors influence resilience, including genetics, personality, the presence of supportive adults, and access to mental health resources. Nonetheless, trauma is one of the most powerful risk factors for adolescent substance misuse.
The severity and timing of trauma also matter – for example, repeated or early-childhood trauma tends to have a greater impact on brain development and risk-taking behavior than a single, later incident. Protective factors such as strong social support, healthy coping skills, and a stable home environment can reduce the risk that a traumatized teen will turn to drugs. Still, when we look at populations of youth, those with significant trauma histories consistently show much higher rates of smoking, drinking, and drug use than those without.
Trauma tilts the odds toward substance use by altering both a teen’s emotional landscape and biological stress systems in ways that make the allure of drugs more potent.
The Co-Occurrence of PTSD and Substance Use Disorders in Teens
Because of the dynamics described above, it is common for serious trauma-related disorders and substance misuse to co-occur in teenage patients. PTSD, the clinical disorder that can develop after trauma, is frequently entwined with adolescent addiction.
Teens with substance use disorders are far more likely to have experienced trauma and to exhibit PTSD symptoms than the general teen population. One clinical study found that adolescent SUD patients had three times higher rates of traumatic events in their histories and five times higher rates of PTSD than non-addicted adolescents in the community.
Correspondingly, youths with PTSD are at high risk for developing substance problems as they try to manage their symptoms – as noted, up to roughly half of teens with addictions also have diagnosable PTSD. This overlap creates a dangerous synergy: each condition worsens the other.
Adolescents burdened with both PTSD and a substance use disorder tend to have more severe addiction severity, worse mental and physical health outcomes, and greater functional impairment than those with addiction alone. They may also face a higher risk of self-harm or suicide, especially if neither issue is adequately treated. Crucially, when trauma and SUD co-occur, treating only the addiction while ignoring the PTSD (or vice versa) is often ineffective.
Experts emphasize that integrated treatment – addressing both the trauma and the substance use – yields better outcomes, as each issue needs to be healed to break the cycle. In fact, trauma-informed care in youth addiction treatment has been shown to improve engagement and reduce relapse, since it helps teens develop healthier coping mechanisms for their trauma triggers instead of returning to drugs.
Conclusion: Breaking the Cycle
The robust link between trauma and teen substance use highlighted by research sends a clear message: preventing and addressing childhood trauma is an essential part of combating adolescent drug and alcohol misuse.
Trauma is not just an emotional wound; it has concrete neurobiological and behavioral effects that can set a teen on a path toward addiction. By the same token, helping young people heal from trauma or PTSD and building their resilience can significantly reduce the likelihood of substance abuse.
This means that parents, schools, and healthcare providers all have a role to play. Recognizing signs of trauma and providing support (such as counseling or trauma-focused therapies) early on can interrupt the trajectory that leads from victimization to self-medication. For teens already using substances, trauma-informed intervention is critical – treatment programs must address the underlying pain fueling the drug use.
As studies show, when teens learn healthier ways to cope with stress and emotional pain, their need for substances as an escape diminishes. In summary, trauma and adolescent substance use are tightly interwoven, but with informed care and prevention efforts, that cycle can be broken. By investing in safe, stable environments and early trauma interventions for our youth, we not only ease their immediate suffering but also reduce the prevalence of addiction down the line. The evidence is clear that addressing trauma is key to fostering a healthier, drug-free future for vulnerable teens.
References
- Compass Health Center. (2024). Teen Mental Health Statistics.
https://compasshealthcenter.net/blog/teen-mental-health-statistics/ - Indian Health Service. (n.d.). Trauma in Children and Adolescents.
https://www.ihs.gov/sites/telebehavioral/themes/responsive2017/display_objects/documents/slides/nationalchildandadolescent/traumainchildren1115.pdf - National Child Traumatic Stress Network. (2023). Making the Connection: Trauma and Substance Abuse.
https://www.nctsn.org/sites/default/files/resources/making_the_connection_trauma_substance_abuse.pdf - Substance Abuse and Mental Health Services Administration (SAMHSA). (2023). The Role of Adverse Childhood Experiences in Substance Misuse Prevention.
https://www.samhsa.gov/sites/default/files/sptac-ace-role-of-substance-misuse-prevention.pdf - ScienceDirect. (2023). Trauma-Related Neurodevelopmental Effects in Adolescence.
https://www.sciencedirect.com/science/article/pii/S0149763423000027 - ScienceDirect. (2016). Adolescent Stress Exposure and Brain Development.
https://www.sciencedirect.com/science/article/pii/S0149763416300811 - Child and Adolescent Psychiatry and Mental Health. (2025). PTSD Prevalence After Trauma in Youth.
https://capmh.biomedcentral.com/articles/10.1186/s13034-025-00879-4 - Zipdo. (2024). Teen Trauma Statistics.
https://zipdo.co/teen-trauma-statistics/ - U.S. Department of Health & Human Services. (n.d.). Data on Trauma and Substance Use in Youth.
https://www.hhs.gov/
More posts like this
.svg)
Guiding your teen’s path to mental clarity, sobriety, and a hopeful future.
For more information or to schedule a visit, please reach out to us today. Our empathetic and caring team is here to support you every step of the way.
.svg)
.avif)
.svg)
.svg)



